“Myia is powering our transition to value by reducing the cost of care and allowing us to reach many more patients across the risk spectrum.
”
CUSTOMER CASE STUDY
THE SITUATION
In 2015, Mercy Health launched the country’s first virtual hospital in St Louis Missouri. With an imperative to perform in value- based arrangements and a vision for how a more preventative and personalized model of care could improve outcomes and reduce the cost of care, the “hospital without beds” foretold a future where the home is the default venue of care.
Mercy’s ambitious “vEngagement” program raised the standard of care for patients living with complex chronic conditions, such as heart failure, COPD, diabetes and hypertension. Their program had reduced unnecessary ED visits and admissions hospital, and lowered the cost of care, with impressive patient satisfaction. Having pioneered such an impactful virtual more of care, Mercy was looking for a new technology partner
to help scale the program to support many more lives under management, without an increase in clinical headcount. Mercy believed that the right technology could achieve this through more automation, efficient clinician-centric virtual workflows, shifting virtual encounters from video to asynchronous communication, and intelligent triage to reduce unnecessary alerts associated with typical Remote Patient Monitoring (RPM).
THE CHALLENGE
Apply Myia’s virtual care technology platform to increase “lives under management” without any increase in clinical headcount, while maintaining clinical outcomes and lower cost of care, with world class patient satisfaction.
The beneficiaries: High-risk co-morbid patients within value-based care contracts living with complex and costly chronic conditions, including: Heart Failure, COPD, Hypertension, and Diabetes.
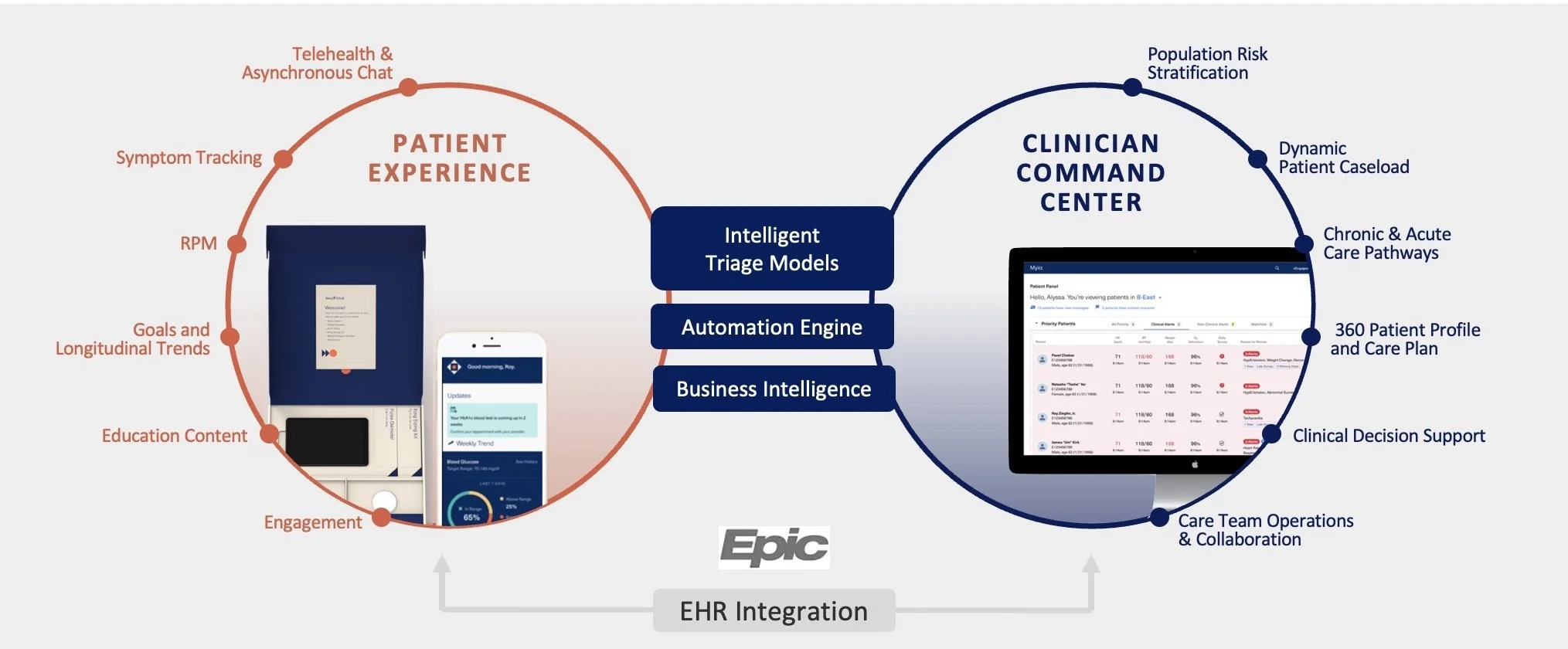
WHAT: THE PLATFORM
Mercy uses the full end-to-end Myia platform and services capabilities, from patient risk stratification, RPM, Machine Learning (ML) triage models, asynchronous communication and bi-directional integration between the Myia Clinician Command Center and Epic.
HOW: THE SCOPE
Migrate over 2,500 complex chronic patients and ~100 clinical users from a basic incumbent RPM solution.
Integrate to Epic to improve workflows and avoid redundant documentation.
Reduce the total cost of ownership for monitoring hardware, logistics, and support.
Apply analytics to personalize engagement and reduce unnecessary alerts.
Implement asynchronous communication to reduce unnecessary video encounters and improve the patient experience.
Provide world class tier 1 and tier 2 patient support.
Apply Myia’s closed loop insights and continuous improvement methodology.
WHY: THE OUTCOMES
Since migrating Mercy Virtual clinicians and their patients to the Myia platform:
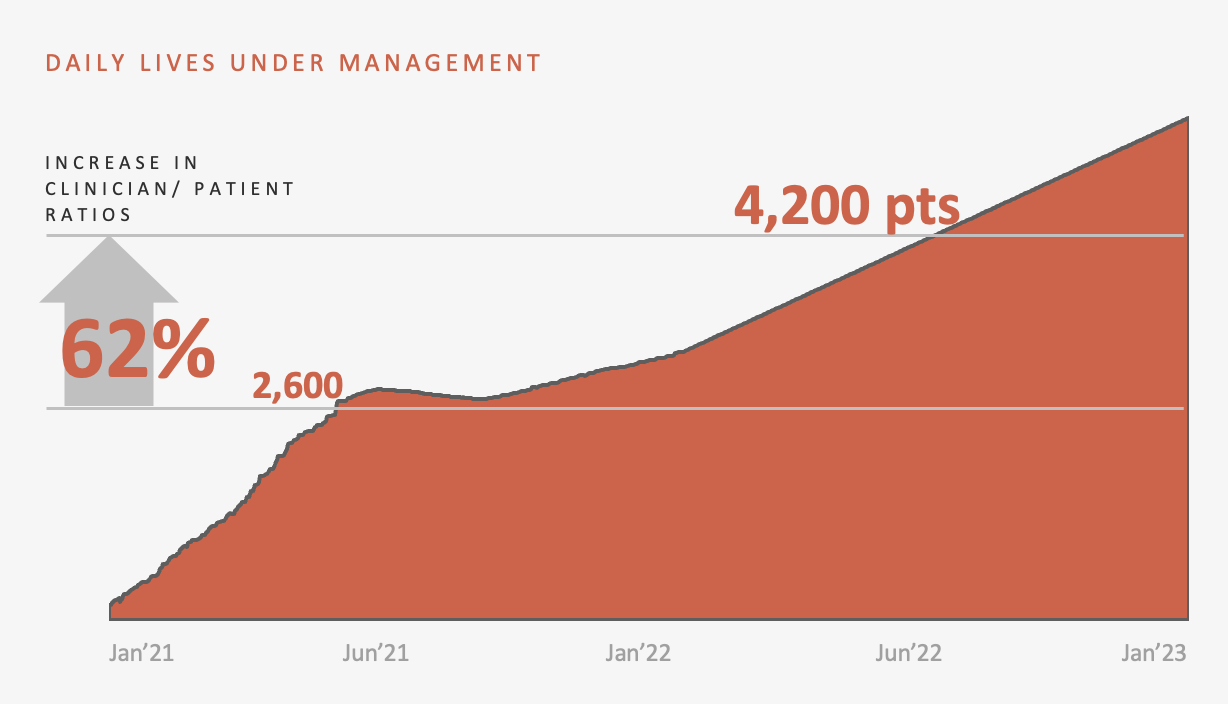
62% increase in patient : clinical ratios, while maintaining a 50% reduction in unnecessary ED visits and admissions
+88 Patient Net Promoter Score (NPS) for the connected care program
89% daily data engagement (vitals collection, symptom surveys)
40% fewer video encounters for teams adopting Myia’s integrated asynchronous chat
53% reduction in TCO for hardware and logistics
1 day average order-to-ship time for home monitoring kits
“Myia has unlocked >60% improvement in clinical staff to patient ratio with a short-term expectation of an additional 50% increase in capacity.”
”
“This program is a godsend.”
+88 NPS
“IT IS SO CONVENIENT TO HAVE ALL THE EQUIPMENT IN THE HOUSE AND NOT HAVING TO RUN TO AND FROM THE HOSPITAL… WE ARE SO VERY APPRECIATIVE OF THE PROGRAM AND THE HELP I HAVE RECEIVED.”
– A PATIENT ON THE MYIA PLATFORM